BARIATRIC SURGERY
Bariatric surgery(from the Greek words "baros," meaning "weight," and "iatrikos," meaning "medicine"). For many people, weight-loss surgery is an effective way to treat their obesity or morbid obesity. If you're thinking about weight-loss surgery, you probably have questions. Get the answers you need to make an informed decision about whether this procedure is right for you.
THREE COMMON TYPES OF PROCEDURES:
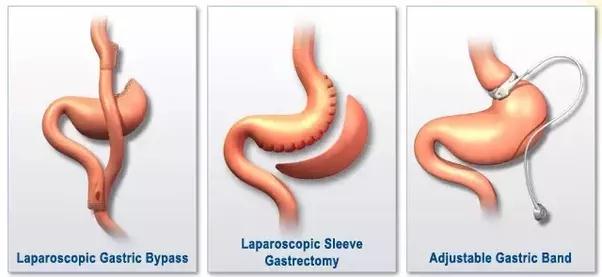
Make informed decisions about your care. Take your time to learn about the various weight loss strategies.
- Restrictive techniques make your stomach smaller.
- Malabsorptive techniques decrease your ability to absorb nutrients from food.
- Sleeve gastrectomy is a restrictive procedure. The surgeon removes two-thirds of the stomach, which provides a quicker sense of fullness and decreased appetite.
- Roux-en-Y gastric bypass is both a restrictive and a malabsorptive procedure. The surgeon decreases the size of your stomach and causes food to go only through part of the small intestines.
- Adjustable gastric banding is a restrictive procedure. The surgeon places a band around the top of the stomach. This limits food intake, thus encouraging weight loss.
-
SLEEVE GASTRECTOMY
This procedure is a restrictive procedure that changes the shape and size of the stomach. The surgeon removes approximately two-thirds of the stomach; thus, the stomach is reshaped into a long tube, or “sleeve.” After the procedure, the stomach is about the size and shape of a banana and resembles a sleeve.
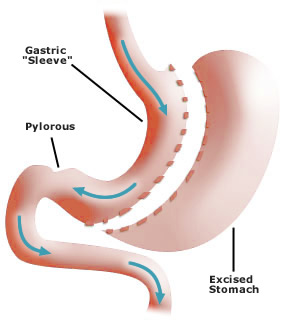
WHY CHOOSE SLEEVE GASTRECTOMY
The procedure:- restricts food intake by allowing only a small amount of food to be consumed in a single sitting, providing a quicker sense of fullness and decreased appetite
- does not require the surgeon to implant a foreign body such as the band used in gastric banding
- decreases the secretion of the hormone ghrelin, which is responsible for the feeling of satiety (fullness)
- initially decreases the body weight of the severely obese patient to prepare this patient for a staged procedure or other surgery at a later time
-
GASTRIC BYPASS
This procedure is both restrictive and malabsorptive. The surgeon converts the stomach to a small pouch that holds approximately 2 ounces of food. The gastric bypass procedure then routes food past most of the stomach and first part of the small intestine. In addition to restricting food intake, a Roux-en-Y gastric bypass reduces nutrient absorption.
This surgery limits the amount of food that can be eaten, yet leaves the patient feeling full and satisfied on very little food. Having less food naturally results in reduced caloric intake, and weight loss usually follows. With Roux-en-Y gastric bypass, risks for nutritional deficiencies are higher than restrictive procedures (bypass causes food to skip the duodenum, where most iron and calcium are absorbed).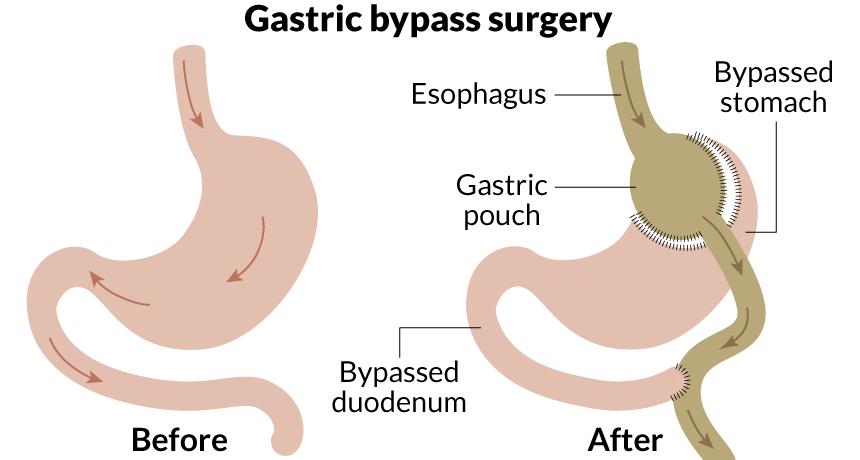
WHY CHOOSE ROUX-EN-Y GASTRIC BYPASS
The procedure:- causes an early sense of fullness and satisfaction, thus reducing the desire to eat
- commonly results in greater weight loss
- requires less long-term maintenance relative to gastric banding (no band fills needed)
- reduces the chance to “cheat” the surgery compared with gastric banding
-
ADJUSTABLE GASTRIC BANDING
This procedure is restrictive. The surgeon places an adjustable band at the top of the stomach to create a small pouch. The band can be adjusted to increase or decrease the restricted area of the stomach through a port. The opening to the rest of the digestive tract is adjustable through an epidermal port.
Weight loss is slower than alternative weight loss procedures, but with appropriate aftercare and routine band adjustments, ultimately results in comparable long-term weight loss 3 or 4 years after surgery. Risks associated with adjustable gastric banding include band erosion or slippage, equipment malfunction, or infection.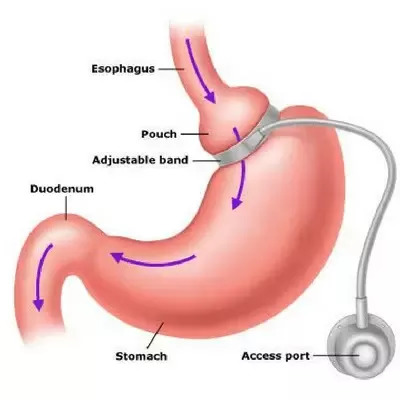
WHY CHOOSE ADJUSTABLE GASTRIC BANDING
The procedure:- makes you feel full after limited food
- does not cause vitamin or mineral deficiencies due to malabsorption
- is less invasive than other procedures
- is reversible
